Pelvic Physiotherapy for Endometriosis: 5 Reasons One Should be on Your Team
By Jill Mueller
Pelvic Health Physiotherapist
Have you heard of Pelvic Physiotherapy; or if you have, did you think it was just for women who need to strengthen their pelvic floor? Well, I’m here to let you know that Pelvic Physiotherapists do more than teach kegels; and if you do have endometriosis you should have one on your team!
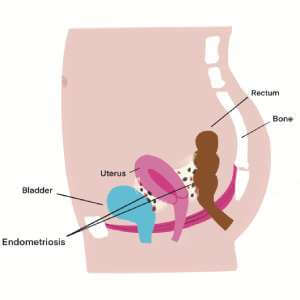
Before we dive into how Pelvic Physiotherapy can help, let’s have a look at what Endometriosis is.
What is Endometriosis?
By definition, endometriosis is a disease that is tissue similar to (but not the same as) the uterine lining found outside of the uterus.1 It affects 10% of the population born with a uterus (190 million people worldwide).2 This is equivalent to asthma and diabetes, and yet it remains drastically under-researched without any known cause, no cure, and an invasive way to diagnose it.
Symptoms
Common symptoms can include:

For a full checklist to bring to your doctor, click here.
The variety of symptom presentation and referral to different healthcare practitioners for the broad range of issues (urology for bladder issues, gynaecology for reproductive pain, gastroenterology for digestive discomfort) all add to prolonged suffering and diagnostic delay.3
Physiotherapists may be the first profession to connect all the dots. It is important for us to become familiar with this disease and help guide our clients to a gynaecologist with a focus in endometriosis to improve management time of this debilitating disease.4
Pelvic Physiotherapy for Endometriosis
Pelvic Physiotherapy includes all things pee, poo, and sex-related! With the complexity of Endometriosis, it often includes all of these.
Here are 5 reasons you should include a Pelvic Physiotherapist on your Healthcare team
1. Bladder Pain
Some people with Endometriosis are also diagnosed with interstitial cystitis (IC) or bladder pain syndrome (BPS). This can be described as a feeling of pain and pressure in the bladder area, or the feeling of a UTI (urinary tract infection) without culturing positive for an infection. There may be a sense of urinary urgency and/or frequency (urinating more than 8x/day).
Endometriosis of the bladder is very rare, but through visceral-visceral (uterus to bladder) or visceral-somatic (pelvic floor to bladder) convergence, the bladder can become sensitized.
Your Pelvic Physiotherapist will have you do a bladder diary and provide education on what foods and drink might be contributing to symptoms. They will check if your pelvic floor and abdominals are squeezed tight which may be adding pressure or irritation to the bladder. If bladder pain is your symptom, Bladder Drill training (where you are progressively exposed to holding more and more urine in the bladder) may be a treatment of choice.
2. Bowel Pain
Endometriosis is often found in the place between the uterus and the rectum (recto-uterine pouch). Adhesions formed here can make it a challenge to have a bowel movement, contributing to constipation or pain, especially during your period. Dyschezia during menses can be strongly predictive of endometriosis.5
Pelvic Physiotherapists love to talk about poo! What goes in impacts what comes out, so your therapist will have a look at your fibre, quality of food and hydration in order to optimize your bowel movement (BM). Assessing your pelvic floor will help determine if it is relaxed enough to pass stool, and advice will be provided on bathroom and bowel habits. Exercise and routine is important for a good BM, as is your stress and anxiety levels. Digestive health is a complex system that depends on a variety of factors. A thorough approach will help guide you to better bowels.

3. Chronic Pelvic Pain (CPP)
Commonly defined as pain in the pelvic area lasting 3 months or longer.6 Endometriosis is the most common cause of CPP.7 Chronic pelvic pain is considered a form of chronic regional pain syndrome, where central sensitization or nociplastic pain is involved. This is when the nervous system becomes sensitized and treatment depends on a multidisciplinary approach.
This is our bread and butter as Pelvic Physiotherapists. I don’t know any Pelvic Physios who don’t have someone in their caseload with chronic pelvic pain. Research in this area shows that using a whole-person, biopsychosocial approach to therapy is the best way to address persistent pain. This means looking at your ability to move and do activity and/or any physical tightness or restrictions (bio-logical); your understanding of pain itself – if you’ve developed any negative thought patterns or fear-avoidance behaviours that might be contributing to your symptoms (psycho-logical). As well as looking at how this is affecting your social behaviours – missing work/school, not going out with friends, avoiding intercourse (social-logical).
4. Pain with Penetration
This can include any penetration (using a tampon, getting a pap exam, or sexual intimacy). Pain with deep penetration can be due to tenderness in the pelvic floor muscles and/or bladder,8 or a lack of mobility of the cervix due to adhesions in the ligaments and fascial pouches around the uterus. Pain with initial penetration is often a protective response and tightening of the pelvic floor muscles occurs in anticipation of discomfort.
If you have an overactive pelvic floor, this is where kegels (pelvic floor strengthening) may actually contribute to worsening of symptoms. If you had tight leg muscles, would you go and do a bunch of squats? No… you would get a massage, stretch and relax the muscles. The pelvic floor muscles are no different! Your Pelvic Physio will teach you how to downtrain and relax the pelvic floor. They may introduce the use of dilator therapy to help guide your body to relax during penetration while you progressively work toward inserting a tampon, speculum or during intercourse.
5. Pain/Flare ups
A flare up can occur when our body, mind and nervous system become overwhelmed. It is our brain’s way of trying to protect us and get us to slow down. But this can be a struggle if you are trying to do your daily activities, stay active and be productive at work and/or as a parent.
This is another area where Physiotherapy excels! A Pelvic Health physiotherapist who is well versed in pain neuroscience can help guide you on pacing and progressing. Learning about listening to your body, and knowing when to push and when to pull back are an important tool to avoiding flare ups, moving toward your goals, and getting back to living the life you want to live.
Endometriosis is a complex disease affecting many aspects of one’s life. If you have Endometriosis, consider adding Pelvic Physiotherapy to your healthcare team!
Healthy Balance Physiotherapy & Wellness is a physio-owned clinic on the border of Oakville and Burlington that has been in business for over 15 years. The team has expanded to include 5 pelvic health therapists who are all well versed in Endometriosis. Led by Jill Mueller, who also has this disease and teaches an Endometriosis course for Pelvic Health therapists, the team at Healthy Balance has developed an integrated Endometriosis Program for patients.
Call to book your free discovery call!
Follow @endotogether

References:
1. World Health Organization (WHO). International Classification of Diseases, 11th Revision (ICD-11) Geneva: WHO 2018.
2. Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med 2020; 382:1244-56.
3. Agarwal SK, Chapron C, Giudice LC, et al. Clinical diagnosis of endometriosis: a call to action. Am J Obstet Gynecol 2019(4):354-64.
4. For a list of gynecologists with a focus in Endometriosis: www.endometriosisnetwork.com.
5. Nnoaham KE, Hummelshoj L, Kennedy SH, et al. Developing symptom-based predictive models of endometriosis as a clinical screening tool: results from a multicenter study. Fertil Steril. 2012 Sep;98(3):692-701.
6. International Classification of Diseases and Related Health Problems, Eleventh Revision (ICD-11)
7. Hickey M, Ballard K, Farquhar C. Endometriosis. BMJ 2014;348:g1752
8. Orr NL, Noga H, Williams C et al. Deep Dyspareunia in Endometriosis: Role of the Bladder and Pelvic Floor. J Sex Med 2018;15:1158e1166

